CHSLD Policy on Elder Abuse
POLICY STATEMENT
In recent years, several actions and awareness campaigns have been carried out to combat elder abuse. Despite these efforts, elder abuse can exist in every setting. Unfortunately, it often goes without being recognized, acknowledged or reported. All too often, victims of abuse or violence don't dare report it or ask for help. In Canada, the prevalence of elder abuse is estimated at 7%. As the population ages, it is estimated that the number of seniors affected by abuse will rise over the next few years.
At CHSLD Wales Inc. the Executive Director, the Director of Nursing and the Director of Administrative Services are responsible for ensuring compliance with this policy and for promoting a culture of well-being within the establishment, as well as taking the necessary steps to prevent any situations of abuse that are brought to their attention. They raise awareness of elder abuse among staff, residents and their families/loved ones. They provide employees and health and social service providers with training and procedures for recognizing, reacting to and intervening in cases of abuse.
SCOPE
This policy applies to all CHSLD Wales Inc. employees, families/loved ones and volunteers, including health and social service providers.
Please note that the Foyer Wales Home, a residence for seniors (RPA), as well as the Wales Home Intermediate Resource (IR), are governed by the CIUSSS de l'Estrie-CHUS’S policy : Politique de lutte contre la maltraitance envers les aînés et toute autre personne majeure en situation de vulnérabilité du CIUSSS de l’Estrie-CHUS (B000-POL-02) and the Procédure de lutte contre la maltraitance envers les aînés et toute autre personne majeure en situation de vulnérabilité du CIUSSS de l'Estrie-CHUS (E000-PROCD-04).
OBJECTIVES
The purpose of this policy is to establish measures to prevent and combat abuse, and to support teams and intervenors in any action taken to put an end to it. More specifically:
- Ensuring the safety, well-being and quality of life of residents according to their needs and respecting their rights;
- Ensuring that no form of elder abuse is tolerated;
- Ensuring that no form of discrimination, such as ageism, is tolerated;
- Providing a caring environment;
- Promoting good treatment with principles and values guiding our actions to prevent and combat abuse;
- Defining each of the steps involved in identifying and managing a situation of abuse;
- Informing and equipping all those concerned with the obligation to report cases of abuse;
- Equipping teams to combat abuse;
- Defining the roles and responsibilities of the individuals involved in preventing and combating abuse;
- Supporting the continuous improvement of clinical practices and the quality of care and services;
- Planning skill development activities to equip employees, stakeholders and managers with best practices;
- Offering the required support and accompaniment to the person presumed to be abused or mistreated, as well as to the family or loved ones if required;
- Ensuring that no form of reprisal is taken against a reporter;
- Implementing and enforcing administrative, disciplinary or other measures when required to stop abuse.
DEFINITIONS
- Well-treatment: Is distinguished by the act of taking the person's point of view into account before any action is taken. When it is impossible to obtain the person's point of view, the person's previously expressed point of view (verbally or in writing) or that of a loved one may be taken into consideration (Plan d'action gouvernemental pour contrer la maltraitance envers les personnes aînées, p.26).
- Benevolence: An attitude that consists in looking after people's well-being. It is expressed in three (3) dimensions: physical, psychological and social. Benevolence creates a climate of security and generalized trust.
- Abuse: A singular or repetitive gesture or failure to act appropriately that occurs in a relationship where there should be trust and that causes, intentionally or unintentionally, harm or distress to a person (Loi visant à lutter contre la maltraitance envers les aînés et toute autre personne majeure en situation de vulnérabilité, art. 2, para. 3);
- Intentional abuse: The abuser wants to harm the older person.
- Unintentional abuse: The abuser does not want to cause harm or does not understand the harm he or she is causing.
- Neglect: Failing to care for the elderly person, by failing to take appropriate action to meet their needs.
- Person in a vulnerable situation: A person of full age whose ability to request or obtain assistance is temporarily or permanently limited, due in particular to a constraint, illness, injury or handicap, which may be of a physical, cognitive or psychological nature, such as a physical or intellectual disability or an autism spectrum disorder (Act to combat elder abuse and any other person of full age in a vulnerable situation, art. 2, para. 4);
- A person working for the establishment: A physician, dentist, midwife, staff member, medical resident, trainee, volunteer or any other individual who provides services directly to a person on behalf of the establishment (Loi visant à lutter contre la maltraitance envers les aînés et toute autre personne majeure en situation de vulnérabilité, art. 2, para. 5);
- Health and social services provider: Any person who, in the performance of his or her duties, directly provides health or social services to a person, on behalf of an establishment, a private seniors' residence, an intermediate resource or a family-type resource, including those who carry out activities described in sections 39.7 and 39.8 of the Professional Code (chapter C-26), as well as the operator or person in charge of the residence or resource, where applicable. (Loi visant à lutter contre la maltraitance envers les aînés et toute autre personne majeure en situation de vulnérabilité, art. 2, para. 6);
- Collaborative intervention process: The collaborative intervention process involves stakeholders from organizations represented by government departments and agencies that are signatories to the national framework agreement in the fields of health and social services, justice and public safety. These organizations intervene with seniors in vulnerable situations to ensure better protection and provide the necessary assistance to those who are presumed abused or abused in a way that may constitute a criminal or penal offence;
- User: Person receiving care or services from the facility, regardless of the health and social services provider;
- Violence: Abusing an older person or making them act against their will, using force and/or intimidation.
NORMATIVE AND LEGISLATIVE FRAMEWORK
- Loi sur la santé et les services sociaux (LSSS);
- Loi visant à lutter contre la maltraitance envers les aînés et toute autre personne majeure en situation de vulnérabilité;
- Professional Code;
- Québec Charter of Human Rights and Freedoms;
- Québec Civil Code.
OTHER DOCUMENTS CONSULTED
- Politique de lutte contre la maltraitance envers les aînés et toute autre personne majeure en situation de vulnérabilité - CIUSSS de l'Estrie-CHUS;
- Procédure de lutte contre la maltraitance envers les aînés et toute autre personne majeure en situation de vulnérabilité - CIUSSS de l'Estrie-CHUS;
- Plan d'action gouvernemental pour contrer la maltraitance envers les personnes aînées 2022- 2027 - Ministère de la Santé et des Services Sociaux;
- Tool to support the development and revision of policies to combat abuse of seniors and other vulnerable adults - Ministère de la Santé et des Services Sociaux;
- Les douze (12) droits des usagers - Regroupement provincial des comités des usagers (RPCU) - Ministère de la Santé et des Services sociaux;
- Preventing abuse for healthy aging - Food for thought - Institut national de santé publique du Québec (INSPQ);
- Guide de référence pour contrer la maltraitance envers les ainées (Cadre de référence), 2e edition, 2016 - Ministère de la Santé et des services sociaux (MSSS).
1. PREVENTION, RAISING AWARENESS AND SKILL DEVELOPMENT:
1.1. Prevention
"The prevention of abuse aims to reduce or even eliminate its incidence in all living environments for seniors or adults in vulnerable situations. It is based on the promotion of values such as respect for human dignity, knowledge of the causes and factors associated with abuse, and the empowerment of all social players in the fight to reduce this social problem. It increases collective awareness and contributes to the acquisition of respectful attitudes and behavior towards the elderly. It creates a climate in which the people concerned feel more comfortable in breaking the silence and taking the necessary steps to counter this abuse." (Guide de référence pour contrer la maltraitance envers les personnes aînées, 2016, p. 23)
Abuse can take the form of violence or neglect and has numerous consequences for the health and well-being of those affected, as well as a social and economic impact in terms of healthcare and loss of contribution by seniors. In addition to causing physical and psychological suffering, it adversely affects seniors' quality of life and contributes to lower life expectancy (INSPQ, 2021, p.3).
1.2. Awareness
In the fight against abuse, raising awareness, prevention and skill development remain effective means of reducing, if not eliminating, the incidence of this phenomenon in all living environments for seniors and other vulnerable adults. Raising awareness and prevention efforts are aimed at both people working for the establishment, health and social service providers, users, family and friends, volunteers and visitors, as it is aimed at the public. In addition, promoting a culture of well-treatment is a positive and promising approach to countering abuse.
CHSLD Wales Inc. several tools and means at its disposal for this purpose, including:
- Promotion of World Elder Abuse Day (June 15);
- Distribution of information tools on user rights and recourse in the event of abuse (pamphlets, posters from the Mistreatment Helpline (LAMAA) and the Complaints Commissioner (CPQS), etc.) or other material on the fight against elder abuse;
- Posting messages on the establishment's website and on social media (e.g. Facebook);.
- Tools to support teams - See annexes;
- Promotional tools deployed in the CHSLD Wales Inc.;
Information meetings initiated by the establishment or on request (e.g. users' committee, ladies auxiliary, vigilance committee, etc.);
1.3. Skills Development
Competency development is based on activities that ensure the acquisition, maintenance or improvement of knowledge, skills, attitudes and behaviors essential to the execution of a job and comply with the requirements of the establishment.
These development activities are based on the best practices documented in this policy. They are modulated according to needs and target audiences, by managers and designated mistreatment intervenors, and can take different forms such as:
- Theoretical training to combat elder abuse,
- Training platform for external service partners in French (ENA - EPC-ENPC)
- Introduction à la lutte contre la maltraitance envers les aînés ou toutes autre personne majeure en situation de vulnérabilité (Id :2255)
- Identification et signalement d’une situation de maltraitance envers un aîné ou toute autre personne majeure en situation de vulnérabilité (Id: 2944)
- Intervention psychosociale dans l
- La lutte contre la maltraitance envers les personnes majeure en situation de vulnérabilité (Id: 10497)
- Supervision et soutien clinique dans la gestion de situations de maltraitance (Id: 10498)
- Prévention et gestion de la maltraitance envers les résidents et résidentes en CHSLD (Id :10515)
- Theoretical training offered by the facility in English (please note that this training is a summary and translation of the content offered on the training platform for external service partners).
- Training platform for external service partners in French (ENA - EPC-ENPC)
- Community of practice;
- Co-development;
- Information session;
- In June, an information session is offered to employees, residents, families and their loved ones on the prevention of abuse.
2. MANAGING SITUATIONS OF MISTREATMENT:
2.1. Consent
Consent is required for all care or interventions unless there is an emergency. "In case of emergency, consent to medical care is not necessary when the person's life is in danger, or his integrity threatened, and his consent cannot be obtained in a timely manner" (Civil Code of Québec, article 13).
In a situation "to prevent an act of violence, including suicide, when there is reasonable cause to believe that a serious risk of death or injury threatens the senior or the person in a vulnerable situation and the nature of the threat inspires a sense of urgency," consent is not required. (Loi visant à lutter contre la maltraitance envers les aînés et toute autre personne majeure en situation de vulnérabilité, article 20.1 al.2)
"Serious injury means any physical or psychological injury that significantly harms the physical integrity, health or well-being of an identifiable person or group of persons." (Loi visant à lutter contre la maltraitance envers les aînés et toute autre personne majeure en situation de vulnérabilité, article 20.1)
If the elderly person does not consent, the caregiver still has recourse at their disposal. They can:
- Contact the Commission des droits de la personne et des droits de la jeunesse;
- Rely on the Act to amend various legislative provisions (known as "Bill 180") with regard to the disclosure of confidential information to ensure the protection of individuals;
- Rely on the Act respecting the protection of persons whose mental state presents a serious danger to themselves or to others (R.S.Q., c. P-38.001);
- Rely on the Loi visant à favoriser la protection des personnes à l'égard d'une activité impliquant une arme à feu et modifiant la loi sur la sécurité dans les sports (L.R.Q., c. P-38.0001), better known as "Loi Anastasia". This law ensures the immunity of professionals who denounce a situation by lifting professional secrecy;
- Implement emergency interim measures with or without court authorization.
2.2. Identification
Identifying potential abuse is everyone's responsibility. It enables us to be proactive in the fight against mistreatment and requires us to be on the lookout for signs and indicators of mistreatment where appropriate. It involves documenting and analyzing indicators and clues and/or risk factors of mistreatment, using clinical judgment and/or detection tools (annexes 1 to 4). This analysis helps to identify potential situations and justify a more in-depth assessment process.
- Clues: Observable facts that need to be assessed to determine whether they are related to a situation of abuse.
- Indicators: Observable facts that indicate a situation of abuse.
Identifying a potentially abusive situation also involves spotting or screening for signs of abuse. Spotting and screening make it possible to take preventive action, reduce the risk of escalation, prevent worsening consequences and intervene in crisis or emergency situations.
- Spotting: Being alert to signs of abuse in order to identify them.
- Detection: Any situation in which a caregiver or professional has reason to believe that a senior may be experiencing abuse. This person can use tools to identify risk factors and/or signs of abuse.
Once the identification stage has been completed, the person conducting the check decides whether there are observable signs of mistreatment that would justify continuing to manage the situation as one of potential abuse. If, in the opinion of the person conducting the verification, the observable signs can be explained and the presence of mistreatment ruled out, the verification is terminated. In other circumstances, if the person conducting the verification is unable to rule out the presence of mistreatment following the verification of observable clues, he/she continues to manage the situation and proceeds with reporting.
To properly identify these situations, it is important to be familiar with the forms (neglect and abuse) and the seven (7) types of abuse (psychological, physical, sexual, etc.) (Annex 4). If a person is unable to make a clinical judgment, he or she must refer the situation to someone who can take charge of it. Finally, the identification of situations of abuse (presumed or confirmed) is important and must be documented in the files.
2.3. Fact-Checking
Fact-checking is carried out by the relevant department or by the Complaints Commissioner in collaboration with the relevant authorities. The way in which fact-checking is carried out may vary according to the situation and context. Regardless of the method used, the person carrying out the verification of facts must always be carried out in consultation with the relevant department(s) and the CPQS. Fact-checking makes it possible to:
- Document and question the people involved and gather documents and facts from various sources about the situation of abuse;
- Assess the extent of the risk and consequences of abuse for the person being abused;
- Analyze and validate all signs and indicators of a mistreatment situation;
- Assess the situation and confirm whether or not a type of abuse has occurred;
- Intervene and ensure the necessary follow-up.
3. REPORTING AND/OR FILING A COMPLAINT:
Reporting is the act of a person (for example, a witness, a person working for the establishment, a volunteer or a relative) reporting a case of abuse suffered by another person (Politique-cadre de lutte contre la maltraitance envers les aînés et toute autre personne majeure en situation de vulnérabilité, MSSS).
3.1. Mandatory reporting
Population covered by mandatory reporting :
- Any user living in a long-term care facility;
- A resident in a vulnerable situation;
- A person who is medically inapt;
- A person under guardianship, curatorship or approved protection mandate.
Any health and social services provider or professional within the meaning of the Professional Code (chapter C-26) who, in the performance of his or her duties or profession, has reasonable cause to believe that a person is being abused, must report the situation directly and without delay to the Complaints Commissioner of CIUSSS de l'Estrie- CHUS. A manager or other colleague cannot report in place of the health service provider or professional concerned. Reporting must be carried out in complete confidentiality, if that is the wish of the reporter. It is up to the provider or professional to decide whether they wish to report to their manager.
Only providers and professionals are subject to mandatory reporting. Anyone else working for the facility is not obliged to report abuse but is encouraged to do so.
|
CIUSSS de l'Estrie-CHUS Complaints Commissioner (CPQS of the CIUSSSE-CHUS) |
|
|
1-866-917-7903 |
|
Incidents/accidents between two users must be reported without delay to the CPQS if the situation meets the definition of mandatory reporting, as well as the definition of abuse. In such situations, an incident/accident report (AH-223) must be completed, and nursing management must ensure that an interdisciplinary team intervention plan is put in place to eliminate this type of abuse and situations.
"The complaint is lodged by the abused user himself or by his representative. The latter can lodge a complaint directly with the CPQS, as stipulated in the Loi visant à lutter contre la maltraitance envers les aînés et toute autre personne majeure en situation de vulnérabilité (RLRQ, c. L- 6.3, section 3, paragraph 3), in accordance with the complaint examination procedure. If the victim is not a user of the facility, the report must be made to The Mistreatment Helpline (Annex 7), whose role is to:
- Receive calls for information or support;
- Offer active listening;
- Assess the situation described and its level of risk;
- Provide information on available resources and recourse options;
- Refer the person to the most appropriate service providers, including the Complaints Commissioner or a designated service provider;
- Carry out, with the person's consent, a follow-up to accompany them on their journey or steps.
|
The Mistreatment Helpline |
|
|
1-888-489-2287 |
|
It should be noted that the police may also be contacted in the event of a criminal act (risk of death or serious injury).
3.2. Mandatory reporting
In the case of non-mandatory reporting, the health and social services provider must report the situation directly to the CPQS, either verbally or in writing, for persons receiving services. For persons not receiving services, the report can be made to the LAMAA helpline. The healthcare provider must comply with the user's consent and respect confidentiality. Non-mandatory reporting must never be made to an immediate superior or to any other person in the establishment. Reporters must be able to remain anonymous if they wish. However, it may be recommended to notify your immediate superior.
3.3. Reporting to the Complaints Commissioner of CIUSSS de L'Estrie-CHUS (CPQS)
The CPQS is responsible for examining user complaints. They are also responsible for handling reports made under this policy.
- The person must immediately report a situation identified as abuse after a primary verification of the facts. This report can be made in writing or verbally to the CPQS of CIUSSS de l'Estrie-CHUS (Annex 6).
|
CIUSSS de l'Estrie-CHUS Complaints Commissionner (CPQS du CIUSSSE-CHUS) |
|
|
1-866-917-7903 |
|
- The CPQS processes mandatory and non-mandatory reports in accordance with the LSSS and the complaints examination system of the Health and social services network (RSSS).
- A report or complaint to the CPQS may be concluded with or without a recommendation. The CPQS concludes without recommendation when, after analyzing the interventions and measures put in place, it deems that they are appropriate and sufficient to put an end to the situation of abuse, or that the victim is protected. Otherwise, the CPQS concludes by making recommendations to the management concerned if, after analysis, it deems that the interventions or measures put in place are inadequate or insufficient to put an end to the situation of abuse or to protect the victim.
- If a user or their representative is not satisfied with the conclusions reached by the CPQS, they may file a second appeal with the Québec Ombudsman.
|
Québec Ombudsman |
|
|
Website: https://protecteurducitoyen.qc.ca |
1-800-463-5070 |
- If the abuse involves a member of staff, the CPQS can ask to be informed of the disciplinary measures taken.
3.4. Process for reporting a situation of abuse
To know the process for reporting a situation of abuse, please refer to the flow chart in Annex 5.
3.5. Recommended timeline when a situation of abuse is reported to a manager
When a manager is informed of a report, it is his or her duty to ensure that the person presumed to have been mistreated is assisted.
- Upon receipt of information:
- Ensure that a report has been made to the Commissaire aux plaintes et à la qualité des services;
- Quickly take note of the facts and analyze the situation;
- Depending on the situation, refer to a qualified professional for assessment and fact-checking, if you have not already done so;
- Validate user consent, if required;
- Ensure that the care or services potentially required by the physical or psychological state of the person presumed to be a victim of abuse are provided;
- Based on the analysis of the situation, apply the procedures required to remove the alleged abuser from the abused person's living environment, if necessary;
- Gather and preserve evidence to facilitate further action;
- Document the situation in the user's file;
- Document the situation in the employee's file, if the employee is presumed to be the abuser.
- Within 24 hours of receiving the information:
- If the information comes from a third party, ensure that a preliminary disclosure is made to the alleged victim of abuse, or inform the case representative or respondent, as appropriate;
- Complete an incident/accident report (AH-223);
- The manager informs his immediate superior;
- The director of the department concerned informs the director of administrative services and Executive Director;
- Maintain communication links with the immediate superior and with those involved in the process;
- Implement an intervention plan to protect the person presumed abused or mistreated;
- Implement actions, interventions or intervention plan to manage the person presumed abused.
- Within 7 days of receiving the information:
- Ensure that a biopsychosocial assessment of the alleged abused person is carried out;
- Review and analyze the file to determine if there have been any incidents or events that could be attributed to the abuse situation;
- Validate whether there were any other potential victims;
- Maintain communication with the various internal and external bodies involved;
- Implement an intervention plan to protect the alleged victim;
- If necessary, contact the regional abuse coordinator or the Elder Abuse Helpline for advice and support.
3.6. Assessment of the abused person’s needs and abilities
The needs assessment is the responsibility of the CHSLD Wales Inc. management. The caseworker must assess the client and obtain all the clinical information needed to identify risk factors (Annex 2) and determine the abused person's needs. This step is important for forming a professional opinion, targeting future interventions and completing the intervention plan. Based on the needs identified during the assessment, the caregiver can refer the resident to other professionals in the facility or to appropriate organizations, if necessary, to obtain a more complete picture of the situation.
The following professional resources are to be taken into account during the evaluation:
- Clinical team: physician, nurse, licensed practical nurse, caregiver.
- Professional team: social worker, occupational therapist, physical rehabilitation technician, nutritionist, recreation technician.
- Legal: administrative services department, lawyer, notary, public curator, Commission des droits de la personne et de la jeunesse (CDPJ), Complaints Commissioner (CPQS), etc;
- Financial: finance department, banking institution, Autorité des marchés financiers (AMF), etc.
3.7. Action and follow-up on confirmed cases of abuse
Several actions are recommended to follow up on for confirmed cases of abuse.
- Follow-up on the intervention plan for the person presumed abused or mistreated
The implementation of the intervention plan to put an end to the abuse and its follow-up are carried out with the abused person or their representative, as well as all the individuals involved.
- Monitor progress with the resident.
Various follow-up measures can be implemented for victims of abuse:
- Be alert to any situation or behavior that could lead to abuse;
- Help residents and/or their representatives to file complaints, if they so wish;
- Refer or orient residents to other authorities, if required and desired;
- Pay particular attention to the needs of the primary caregiver and offer services where appropriate (respite, etc.).
- Enhancing resident protection.
In addition to mandatory reporting, other protective measures may be considered, such as:
- Opening a legal protection plan;
- Securing assets;
- Ensuring the safety of people in their living environment;
- Take care of the physical and psychological condition of the abused person.
- Follow-up on the intervention plan for the suspected abuser or abused person:
- If the person suspected of being abusive or the abuser is a user of the facility, the intervenor must ensure that an intervention plan is put in place and followed up on.
- If the person is a member of staff, please refer to section 5. PENALTIES.
4. SUPPORT MEASURES
Working in a context of abuse can be complex, requiring interprofessional or intersectoral collaboration to optimize the efficiency of short, medium or long-term interventions. The managers and/or stakeholders responsible for the fight against elder abuse are the people to whom employees, families, loved ones or residents can turn for help in reporting elder abuse or filing complaints. These people can:
- Assist the person in any steps taken to file a complaint with an authority;
- Establish a relationship of trust with the person;
- Identify and recognize signs of abuse;
- Denounce and take a stand against situations of abuse;
- Act according to risk;
- Carry out and collaborate in the assessment of the person's physical and functional autonomy;
- Carry out and collaborate in the assessment of the person's aptitude;
- Provide information on how the complaint system works;
- Inform the resident, family member, friend or employee about the resources and steps that can be taken to report abuse;
- Help the person to clarify the subject of the complaint and/or to draft it, and/or assist and support them at every stage of the process;
- Facilitate conciliation with any relevant body;
- Contribute to the respect of user rights;
- Refer the person to professionals for more specific support if necessary;
- Offer support and listen to the person;
- Establish and maintain contact with the person;
- Remain vigilant for recurring abusive behavior.
4.1. Key intervenors
Resources are available to provide input and support to either the alleged victim, the abuser, witnesses of elder abuse or any other person implicated in the situation.
- The social worker;
- Clinical managers;
- Directors (clinical, administrative and Executive);
- The regional coordinator specialized in elder abuse;
- The Complaints Commissioner (CPQS);
- Le protecteur du citoyen
- The various government agencies accessible via PIC;
- The Mistreatment Helpline (LAMAA): 1-888-489-ABUS (2287);
- Autorité des marchés financiers;
- The Public Trustee
- The Commission des droits de la personne et des droits de la jeunesse;
- The police.
5. PENALTIES
Criminal penalties may apply in the following cases:
- It is an offence to fail to report abuse without delay.
- Anyone who commits an act of mistreatment against a person in a long-term care facility, on these premises or while travelling. A person who, in the performance of his or her duties, commits an act of mistreatment towards a resident of full age to whom he or she directly provides home health or social services on behalf of an institution.
- Anyone who threatens, intimidates, or retaliates against a person who complies with this law, exercises a right granted by it, or reports a violation of it, commits an offense.
- Anyone who hinders or attempts to hinder in any way the performance of the duties of an inspector or investigator.
In accordance with CHSLD Wales Inc. policies and procedures, as well as the Code of Ethics, disciplinary or administrative actions may be applied. For example:
- Examples for employees (including trainees): warnings, letters to file, suspension or dismissal.
- Examples for managers: dismissal, non-reengagement, termination of engagement, suspension without pay, demotion.
- Example for volunteers: termination of contract.
A professional order may impose the following disciplinary actions on one of its members: reprimand, temporary or permanent dismissal, fines, revocation of the permit, revocation of the specialist's certificate, limitation or suspension of the right to engage in professional activities.
The nature of sanctions may vary according to the context and the people involved in the situation. Sanctions may be imposed on the establishment, for example, the appointment of observers, investigations, the requirement to submit an action plan, provisional administration of the establishment, suspension or revocation of a license.
5.1. Procedure for requesting an investigation that may lead to criminal sanctions
To request an investigation that could lead to a criminal sanction, you can:
- Call a responsible person at 1-877-416-8222;
- Submit the completed form "Formulaire de demande d’une sanction pénale en lien avec la maltraitance" available in french only, online:
(https ://cdn-contenu.quebec.ca/cdn-contenu/adm/min/sante-services-sociaux/documents- adm/coordonnees/demande-sanction-penale-maltraitance_mai-2023.pdf):
- by e-mail: die@msss.gouv.qc.ca
- or by mail:
|
Inspection and Investigation Department Ministry of Health and Social Services 3000, avenue Saint-Jean-Baptiste, 2nd floor, local 200 Québec (Québec) G2E 6J5 |
- You can also make a declaration online (https://www.quebec.ca/famille-et-soutien-aux-personnes/violences/maltraitance-aines-personnes-vulnerables/formulaire-maltraitance)
For more information on applying for penal sanctions, visit the following website: Québec.ca (https://www.quebec.ca/gouvernement/ministere/sante-services-sociaux/coordonnees/coordonnees-supplementaires-du-ministere-de-la-sante-et-des-services-sociaux)
6. CONFIDENTIALITY
Confidentiality is sometimes seen as an obstacle in the intervention process. It is for this reason that it's important to make a few distinctions and present some guidelines.
6.1. Professional secrecy
In order for the information revealed to be protected by professional secrecy, the person consulted must be a member in good standing of a professional order duly recognized by the Professional Code, which implies the following two conditions:
- Their professional order is recognized under the Professional Code;
- The person consulted was in fact a member in good standing of this professional order at the time the confidences were made.
Note that people working for a professional order are bound by their employer's professional secrecy.
6.2. Confidentiality
The holder of the right to confidentiality is the resident, so the basic rule for disclosure is to obtain their consent. The CPQS must take all necessary measures to ensure that the confidentiality of information identifying a person making a report is preserved, except with that person's consent. The Complaints Commissioner may, however, communicate the identity of this person to the police force.
7. FORBIDDING RETALIATION
The Act to Combat Elder Abuse and Maltreatment of Seniors and Other Vulnerable Persons of Full Age contains several important elements concerning the prohibition of reprisals against those who report abuse.
“It is prohibited to retaliate against a person who, in good faith, makes a complaint or report or cooperates in the examination of a complaint or the processing of a report. It is also forbidden to threaten a person with reprisals for refraining from making a complaint, reporting a matter or cooperating in the examination of a complaint or the processing of a report. The demotion, suspension, dismissal or relocation of a person, as well as any disciplinary sanction or other measure affecting his or her employment or working conditions, are presumed to be retaliatory measures. Displacing a resident, breaking his or her lease or prohibiting or restricting visits to the resident are also presumed to be measures of reprisal”. (Article 22.2)
“A person may not be prosecuted for having, in good faith, formulated a complaint, made a report or cooperated in the examination of a complaint or the processing of a report, regardless of the conclusions reached." (Article 22.3)
8. CPQS ANNUAL REPORT
“The service quality and complaints commissioner must, in the report on his or her activities, include a section dealing specifically with complaints and reports he or she has received concerning cases of abuse of seniors and people in vulnerable situations, without compromising the confidentiality of reporting files, including the identity of the persons concerned by a complaint or report.” (Loi visant à lutter contre la maltraitance envers les personnes aînées et toutes autres personnes majeures en situation de vulnérabilité, article 14).
9. ROLES AND RESPONSIBILITIES
Board of Directors:
- Adopt this policy to combat elder abuse.
Vigilance Committee:
- Follow-up on recommendations relating to the handling of reports of abuse.
- Carry out any other duties the Board of Directors deems appropriate in connection with this policy and in keeping with its mandate.
Users' Committee:
- Support the application of this policy.
Executive Director:
- Ensure the policy or any amendments to the policy adopted by the Board of Directors;
- Ensure that the facility's policy is reviewed every five (5) years;
- Ensures compliance with this policy;
- Integrate values that foster a culture of respect, transparency and continuous improvement;
- Ensure that the necessary changes are made to remedy any difficulties in implementing and improve procedures and practices;
- Report on the handling of reported cases of abuse;
- Ensure that an abuse awareness and training plan for everyone working for the facility is developed and implemented;
- Ensure that reporting procedures are clear and known to all persons who may receive reports within the facility;
- Ensure that strategies to ensure confidentiality and protection against retaliation for reporting are established and implemented;
- Ensure that a policy dissemination plan is developed and implemented;
- Ensure that the policy is accessible to all by posting in public view and on the facility's website;
- Ensure that the policy is known to all residents and their families.
- Make staff and managers aware of the importance of a culture of kindness and the existence of this policy from the moment they are hired;
Director of Quality and Administrative Services:
- Monitor the application of this policy in collaboration with the Director of Nursing and the designated worker at CHSLD Wales Incs.;
- Integrate values that foster a culture of respect, transparency and continuous improvement;
- Support individuals in the dissemination and application of this policy;
- Ensure staff and managers are aware of the importance of a culture of well-being and the existence of this policy from the moment they are hired;
- Provide all staff with the necessary training on abuse, according to their role within the facility, in collaboration with other directors and the designated person responsible for combating abuse;
- Support managers in applying appropriate intervention and follow-up measures when the perpetrator of abuse is a member of the facility's staff;
- Collaborate in identifying and applying recommendations or sanctions when dealing with a report involving a person working for the establishment.
- Where applicable, inform the facility's lawyer of any disciplinary measures taken as a result of the processing of the file submitted for disciplinary review when the perpetrator of the abuse is a member of the facility's staff;
- Report on the handling of reported cases of abuse;
- Ensure that appropriate intervention and follow-up measures are applied when the perpetrator of the abuse is a volunteer from the CHSLD Wales Inc. volunteer team;
- Where applicable, inform the lawyer of the measures taken following the processing of the file submitted for review when the perpetrator of the abuse is a volunteer.
Director of Nursing/Person responsible for policy implementation (PRMOP):
- Assume the role of person responsible for policy implementation (PRMOP);
- Submit the policy to the MSSS within 30 days of its adoption by the Board of Directors;
- Make the necessary changes to remedy implementation difficulties and improve procedures and practices;
- Develop and implement an abuse awareness and training plan for all staff working for the facility;
- Ensure that reporting procedures are clear and known to all persons who may receive reports within the facility;
- Establish and implement strategies to ensure confidentiality and protection against retaliation for reporting;
- Develop and implement a policy dissemination plan;
- Make the policy accessible to all by posting in public view and on the company's website;
- Communicate the policy to all users and their families;
- Integrate values that foster a culture of respect, transparency and continuous improvement;
- Responsible for the development and revision of this policy every five (5) years;
- Support individuals in the dissemination and application of this policy;
- Make staff and managers aware of the importance of a culture of kindness and the existence of this policy from the moment they are hired;
- Provide staff with the tools and support they need to meet the specific needs of the clientele concerned at every stage of intervention and follow-up to a situation of abuse;
- Support managers in determining the conditions of application of the reporting obligation and ensure that reporting has been carried out;
- Identify and apply strategies to help identify situations of abuse;
- Support managers in applying appropriate intervention and follow-up measures when the perpetrator of the abuse is a member of the facility's staff;
- Report on the handling of reported cases of abuse;
Unit Managers:
- Promote coordination and collaboration between the various players involved in applying this policy;
- Designate the person(s) who should receive the necessary training to ensure proper and complete management of a maltreatment situation when required;
- Encourage the team to embody the values of the anti-maltreatment policy and foster a culture of good treatment among residents;
- Support staff in applying this policy;
- Ensure prompt intervention in the event of a situation presenting a serious risk of damage to integrity;
- Apply appropriate intervention and follow-up measures when the perpetrator of the abuse is a member of staff reporting to it;
- Educate volunteers about the importance of a culture of care and the existence of this policy.
Healthcare professionals and other intervenors:
Depending on his or her expertise and role in the facility, the intervener may be required to:
- Report any situation that meets the reporting criteria to the Complaints Commissioner (CPQS), for people covered by the application of the policy, and in other cases to a designated intervener through The Mistreatment Helpline (LAMAA);
- Foster a culture of kindness among residents;
- Identify potential abuse situations;
- Carry out fact-finding when a potential abuse situation is identified;
- Assess the needs and abilities of the victim of abuse;
- Ensure diligent follow-up of the intervention to put an end to a situation of abuse;
- Ensure that file management complies with applicable standards;
- Adopt intervention strategies appropriate to the person's profile and the form of abuse;
- Cooperate in the application of this policy;
- Educate volunteers about the importance of a culture of care and the existence of this policy.
Social worker:
- Identify potential abuse situations;
- Responsible for reporting any situation that meets the reporting criteria to the Complaints Commissioner (CPQS), for people covered by the application of the policy, and in other cases to a designated intervener through The Mistreatment Helpline (LAMAA);
- Cooperate in the application of this policy and procedure;
- Participate in the various stages of the abuse management continuum, depending on the need, the expertise required and the relationship with the resident.
10. FINAL REVISIONS
The establishment must adopt a policy to combat abuse of seniors and people in vulnerable situations who receive health and social services, whether these services are provided by the establishment or at home (Article 3 of the law).
The policy must be submitted by the establishment, within 30 days of its adoption, to the Ministry of Health and Social services (MSSS), which, on the recommendation of the Minister responsible for Seniors, approves it within 45 days of its receipt, with or without modification (Section 4.2 of the Act).
The policy must be revised and submitted by the establishment to the Minisstry of Health and Social services (MSSS) no later than every five (5) years, before the date set by the Minister. On the recommendation of the Minister responsible for Seniors, the Minister approves the revised policy, with or without amendments, within 90 days of receipt (Section 7 of the Act).
10.1. Promotion & Policy dissemination
The establishment must post its policy in public view in the facilities it maintains and publish it on its website. It must also, by any other means it determines, make its policy known to it’s residents covered by the policy (CHSLD & RI), including those receiving homecare services, and to significant members of their families (Article 5).
Please note that the Foyer Wales Home, a residence for seniors (RPA), and the Wales Home Intermediate Resource (RI) are governed by the CIUSSS de l'Estrie-CHUS Politique de lutte contre la maltraitance envers les aînés et toute autre personne majeure en situation de vulnérabilité of the CIUSSS de l’Estrie- CHUS (B000-POL-02) and the Procédure de lutte contre la maltraitance envers les aînés et toute autre personne majeure en situation de vulnérabilité of the CIUSSS de l’Estrie-CHUS (E000-PROCD-04).
ANNEXE 1
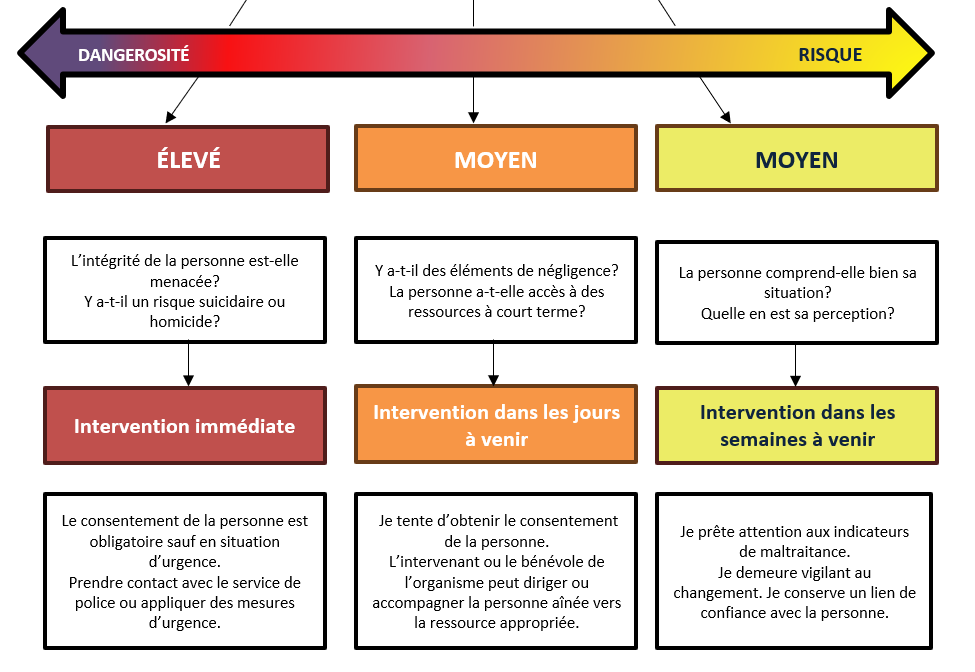
Logigramme – Guide de repérage
Repérer les indices
Les faits : une situation chez la personne aînée me préoccupe
Valider les indices
Je valide les indices avec la personne aînée ou avec une personne visée.
Appréciation du risque
Une intervention est-elle nécessaire immédiatement, dans les jours à venir ou dans les semaines à venir?
Je consulte le responsable de mon organisme ou mon supérieur immédiat.
ANNEXE 2
Facteurs de risques et de vulnérabilités
Facteurs de risque
|
Facteurs de risque en milieu d’hébergement |
||
|
Propre à la personne aînée |
Propres aux membres du personnel |
Propres aux relations |
|
|
|
Facteurs de vulnérabilité
|
Facteurs de vulnérabilité en milieu d’hébergement |
|
Propre à la personne aînée |
|
Facteurs de protection
|
Facteurs de protection en milieu d’hébergement |
|
|
Propre à la personne aînée |
Propres à l’environnement |
|
|
ANNEXE 3
Indices observables selon les types de maltraitances
|
Type de maltraitance |
Indices observables |
|
Maltraitance physique |
Blessures inexpliquées, manque de correspondance entre les blessures et les explications (réponses évasives ou défensives), ecchymoses, grand nombre d’incidents et d’accidents, peur, tremblement, isolement, réticence à recevoir des soins, difficulté à voir la personne aînée seule, absence ou bris de lunettes et prothèses dentaires, sur-médication ou sous-médication, manque d’hygiène, malnutrition, déshydratation, perte de poids inexpliquée, apparence physique négligée (ongles longs, cheveux mal entretenus, etc.), vêtements souillés ou inappropriés pour la saison, maladie physique mal contrôlée, anxiété et angoisse en présence de la personne maltraitante, symptômes dépressifs, agitation, etc. |
|
Maltraitance sexuelle |
Sentiment de honte, repli sur soi, peur, changement de comportement, angoisse ou agressivité au moment des soins d’hygiène ou du changement de vêtements, infections ou plaies aux organes génitaux, douleurs abdominales, désinhibition sexuelle, insomnie, anxiété, symptômes dépressifs, agitation, questionnement de la personne aînée maltraitée sur les pratiques sexuelles de son conjoint ou de sa conjointe, etc. |
|
Maltraitance psychologique |
Peur, culpabilité, repli sur soi, faible estime de soi, nervosité apparente en présence de la personne maltraitante, symptômes dépressifs, confusion ou symptômes d’atteintes cognitives non diagnostiquées, hyperactivité ou hypoactivité, manque d’attention et d’interaction sociale, sécurité insuffisante, milieu de vie non adapté à la condition de la personne, apathie, culpabilité excessive, troubles du sommeil, troubles de la mémoire, changement de comportement, etc. |
|
Maltraitance matérielle ou financière |
Fonds insuffisants pour payer les factures, perte de contrôle sur les finances, disparition de documents liés aux avoirs de la personne, niveau de vie ou services inappropriés malgré des revenus suffisants, disparition d’objets, anxiété lorsqu’on questionne la personne relativement à la gestion de ses avoirs, prêts à des tiers, transactions inhabituelles dans les comptes bancaires, signatures suspectes sur les chèques ou d’autres documents, changement d’institution financière, endettement inexpliqué, changement dans les placements (transactions inhabituelles, rachats massifs ou multiplication des transactions), visite régulière d’un proche à l’occasion de la réception des revenus mensuels, changement soudain de la procuration ou du testament, changement de bénéficiaire dans une police d’assurance-vie, vente de biens, biens personnels ou argent qui ont disparu, etc. |
|
Violation des droits |
Insécurité, difficulté à prendre une décision, privation de relation sociale, refus de fréquenter une ressource, non-accès aux documents légaux, aliénation familiale et sociale, isolement, dénigrement, difficulté pour la personne aînée à rester seule en présence de tiers sans la présence de la personne maltraitante qui tente de contrôler la situation (répond à la place de la personne aînée et ne permet pas de vie privée), contrôle des fréquentations (répond au téléphone à sa place en affirmant que la personne dort, renvoi des amis venus visiter la personne…), etc. |
|
Maltraitance organisationnelle |
Réduction de la personne à un numéro, prestation de soins ou de services selon des horaires plus ou moins rigides, attente indue pour recevoir un service, détérioration de l’état de santé (plaies, dépression, anxiété, etc.), plaintes, etc. |
|
Âgisme |
Langage infantilisant envers la personne aînée, non-reconnaissance des savoirs ou des compétences, exclusion sociale, rejet des idées et du point de vue, honte, culpabilité de ne pas être « à la hauteur », faible estime de soi, insécurité, etc. |
ANNEXE 4
Outil Aide-mémoire – SEPT (7) Types de maltraitance & conséquences
1. Psychologique : Attitudes, paroles, gestes ou défaut d’actions appropriées qui constituent une atteinte au bien-être ou à l’intégrité psychologique.
|
Négligence |
Violence |
Indices |
|
|
|
2. Physique : Attitudes, paroles, gestes ou défaut d’actions appropriés, qui portent atteinte au bien-être ou à l’intégrité physique.
|
Négligence |
Violence |
Indices |
|
|
|
3. Sexuelle : Attitudes, paroles, gestes ou défaut d’actions appropriées à connotation sexuelle non consentis, qui portent atteinte au bien-être ou à l’intégrité sexuelle.
|
Négligence |
Violence |
Indices |
|
|
|
4. Matérielle ou financière : Obtention ou utilisation frauduleuse, illégale, non autorisée ou malhonnête des biens ou des documents légaux de la personne, absence d’information ou mésinformation financière ou légale.
|
Négligence |
Violence |
Indices |
|
|
|
5. Violation des droits : Toutes atteintes aux droits et libertés et sociaux.
|
Négligence |
Violence |
Indices |
|
|
|
6. Organisationnelle : Toute situation préjudiciable créée ou tolérée par les pratiques ou les procédures d’organisations (privées, publiques ou communautaires) responsables d’offrir des soins ou des services de tous types aux personnes aînées.
|
Négligence |
Violence |
Indices |
|
|
|
7. Âgisme : Discrimination en raison de l’âge par des attitudes hostiles ou négatives, des gestes préjudiciables ou de l’exclusion sociale.
|
Négligence |
Violence |
Indices |
|
|
|
Conséquences de la maltraitance
|
Maltraitance physique |
Séquelles physiques temporaires ou permanentes, détérioration de l’état de santé, augmentation de la morbidité et de la mortalité, insomnie, augmentation du recours à l’urgence. |
|
Maltraitance psychologique |
Sentiment croissant d’insécurité, repli sur soi-même, diminution de l’estime de soi, développement d’anxiété, de confusion, tristesse, honte, culpabilité, méfiance, perte de jouissance de la vie, comportements suicidaires ou destructeurs. |
|
Maltraitance financière |
Perte de biens ou d’objets, privation de biens essentiels, perte des épargnes prévues pour assurer son bien-être, précarité, dette, insolvabilité, faillite. |
|
Maltraitance sociale |
Isolement, solitude, perte de contact avec des personnes de l’entourage accroissement de la dépendance, un sentiment d’inutilité sociale. |
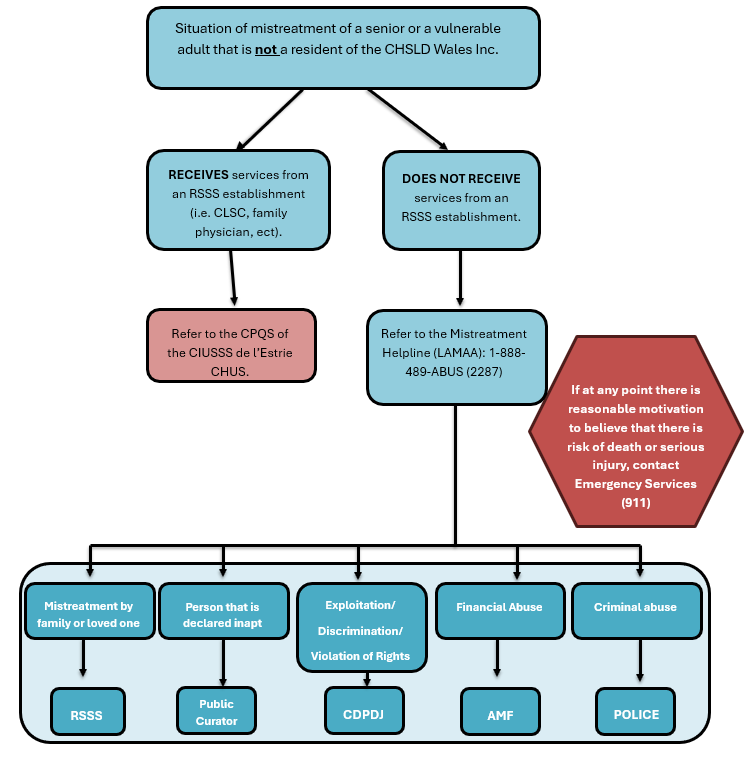
ANNEX 5
Diagram – Mandatory vs. Non-Mandatory Reporting
ANNEX 6
CIUSSS DE L’ESTRIE-CHUS Complaints and Service Quality Commissioner (CPQS) Reporting Form
|
1. Date of report: |
|
|
|
2. Last name, first name of alleged victim: |
|
|
|
3. File number: |
|
|
|
4. Place of residence and street address |
506 route 243 North Cleveland, Québec J0B 2H0 |
☐ CHSLD ☐ RI ☐ RPA |
|
5. Telephone number: |
|
|
|
6. Name of victim’s representative: |
|
|
|
7. Alleged abuser: |
|
|
|
8. Type of mistreatment: ☐ Psychological ☐ Physical ☐ Sexual |
☐ Material or financial ☐ Organizational ☐ Violation of rights ☐ Ageism |
|
|
9. Is the resident under a legal protection order or homologated mandate? |
☐ Guardianship ☐ Public Curator ☐ Homologated mandate |
|
|
10. Description of facts and dates of events:
|
||
|
11. Interventions carried out since the initial event(s):
|
||
|
12. Interventions to come in the near future:
|
||
|
13. Is a manager informed of the situation? If yes, enter the name of the manager. |
|
|
|
14. Is the alleged abuser an employee of the CHSLD Wales Inc? If so, has the HR department been informed? If yes, enter the name of the agent and/or manager. |
|
|
|
15. First name, last name and job title of the person making the report: |
|
|
|
16. Telephone number: |
|
|
|
17. E-mail address: |
|
|
|
18. Date of report: |
|
|
If you don’t have enough room to write the information, you can attach another sheet and number each page please.
Please send the document to plaintes.ciussse-chus@ssss.gouv.qc.ca or call 1-888-917-7903.
ANNEX 7
CONTACT INFORMATION FOR RESOURCE PERSONS
|
Wales Home Resource Persons – Contact information 506 route 243 North, Cleveland QC J0B 2H0 |
|
|
Brendalee Piironen, Executive Director |
819-826-3266, ext. 247 |
|
Chantal Richer, Director of Administrative Services |
819-826-3266, ext. 274 |
|
Audrey Beauchesne, Director of Health Services and responsible for implementing the policy (PRMOP) |
819-826-3266, ext. 224 |
|
Aysa-Renée Goyer, Unit Manager Norton 1 & 2 |
819-826-3266, ext. 287 |
|
Karine Dumont, Unit Manager Norton 3 and professionals, on-call and float teams |
819-826-3266, ext. 288 |
|
Patrick Nolan, Technical Services Manager |
819-826-3266, ext. 226 |
|
Resource Persons at CIUSSS de l’Estrie-CHUS |
|
|
Regional coordinator speciliazed in elder abuse Direction des services multidisciplinaires - Qualité et évolution de la pratique, CIUSSS de l’Estrie-CHUS 50, rue Camirand Sherbrooke (Québec) J1H 4J5 |
819-345-1860 |
|
Complaints Commissioner (CPQS) |
1-866-917-7903 |
|
Protecteur du citoyen Site web: https://protecteurducitoyen.qc.ca Courriel: protecteur@protecteurducitoyen.qc.ca |
Toll free: 1-800-463-5070 QC City Office: 418-643-2688 MTLl office: 514-873-2032 |
|
External Resources |
|
|
The Mistreatment Helpline (LAMAA) https://lignemaltraitance.ca/fr |
1-888-489-2287 |
|
L'Appui, Caregivers https://www.lappui.org |
1-855-852-7784 |
|
SOS Aînés Maltraitance (SOSAM) https://sosam.info |
514-503-5216 |
|
Human Rights and Youth Rights Commission (CDPDJ) |
1-800-361-6477 |
|
Public Curator https://www.curateur.gouv.qc.ca |
1-844-532-8728 |
|
Québec Ombudsman https://protecteurducitoyen.qc.ca |
1-800463-5070 |
|
Autorité des marchés financiers https://lautorite.qc.ca |
1-877-525-0337 |
|
Sureté du Québec https://www.sq.gouv.qc.ca |
911 |
